There is currently a big push from the federal government to open schools this fall. Is this the right move for the country?
There are seven different known types of coronavirus in the world.
Common human coronaviruses
- 229E (alpha coronavirus)
- NL63 (alpha coronavirus)
- OC43 (beta coronavirus)
- HKU1 (beta coronavirus)
Other human coronaviruses
- MERS-CoV (the beta coronavirus that causes Middle East Respiratory Syndrome, or MERS)
- SARS-CoV (the beta coronavirus that causes severe acute respiratory syndrome, or SARS)
- SARS-CoV-2 (the novel coronavirus that causes coronavirus disease 2019, or COVID-19)
The four common ones (229E, NL63, OC43, and HKU1) generally cause symptoms related to the common cold, although they can get into the lower respiratory tract and cause pneumonia. Most people get infected by one or more of these over the course of their lifetime. These viruses are responsible for about 15% of colds. Most children will have at least 6 to 8 colds a year. Children who attend daycare will have more.
Causes of the transmission of colds
- Less resistance. A child’s immune system is not as strong as an adult’s when it comes to fighting cold germs.
- Winter season. Most respiratory illnesses happen in fall and winter, when children are indoors and around more germs. The humidity also drops during this season. This makes the passages in the nose drier and at greater risk for infection.
- School or daycare. Colds spread easily when children are in close contact.
- Hand-to-mouth contact. Children are likely to touch their eyes, nose, or mouth without washing their hands. This is the most common way germs are spread.
Think about this in relation to COVID-19. EVERY ONE of these factors also places children at risk of infection with COVID-19 in a school setting.
This is not just limited to elementary age children. For example, this summer, a high school age team of baseball players led to an outbreak of at least 39 COVID-19 cases in their community, seven of which were team members and one was the coach. The Yamhill County Health and Human Services director stated, “It is suspected that the initial case was contracted when some of the players traveled out of state for a game. This spread further when the team traveled together on a team bus. After this point, several players attended multiple social gatherings prior to knowing they were exposed, which spread COVID-19 beyond the individuals on the baseball team.”
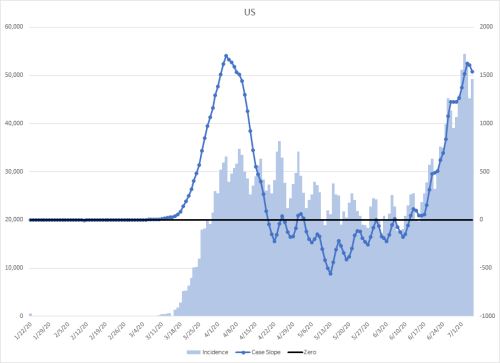
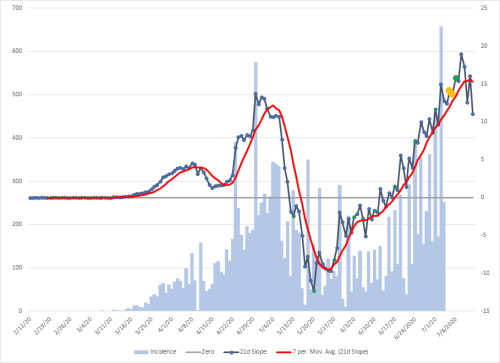
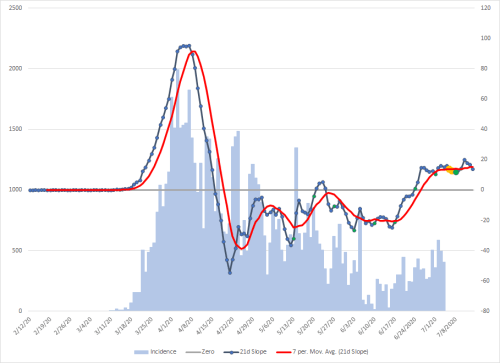
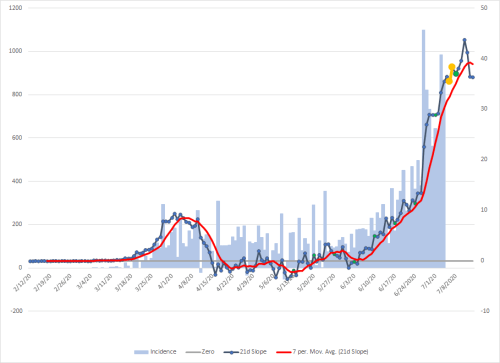
The Data
The Imperial College of London has modeled outcomes of disease by age group. The table below mapped that data to US Census Bureau data to calculate hospitalization and death outcomes. Unfortunately, there was not enough data at the time of publication to estimate the risks to children under 10 years of age.
Assuming that opening schools would spread COVID-19 to just 5% of the population, the impact numbers are pretty staggering, but this is just a model.
| Age | Hospitalizations | ICU Admissions | Deaths |
| 10-19 | 6,491 | 325 | 130 |
| 20-29 | 25,916 | 1,296 | 1,728 |
| 30-39 | 65,010 | 3,250 | 1,625 |
| 40-49 | 130,065 | 8,194 | 3,307 |
| 50-59 | 216,374 | 26,398 | 12,728 |
| 60-69 | 246,067 | 67,422 | 32,611 |
| 70-79 | 204,520 | 88,353 | 42,924 |
| 80+ | 155,151 | 110,002 | 52,854 |
| TOTAL | 1,049,594 | 305,240 | 147,906 |
The outcomes are far worse when using published data. A large data set of 73,214 patient records from the China CDC was mapped to US Census Bureau data. In this data, hospitalization was only broken down into mild, severe, and critical, but not by age, so only totals are provided. I’m assuming that mild means recovery at home, severe means hospitalization, and critical means ICU care.
Mild: 10,993,990
Severe: 1,900,196
Critical: 678,641
The study did break down deaths by age category though
| Age | Deaths |
| 10-19 | 4,327 |
| 20-29 | 4,319 |
| 30-39 | 4,063 |
| 40-49 | 8,818 |
| 50-59 | 27,577 |
| 60-69 | 53,364 |
| 70-79 | 67,332 |
| 80+ | 84,111 |
| Total | 253,911 |
Of course, this is assuming that the disease ONLY spreads evenly within 5% of the population. We know that large spread leads to exponential spread. Given that 70% of the population must be immune for herd immunity and that we don’t know if there is long-term immunity after illness, this is a VERY conservative estimate of the outcome of opening schools.
“The science should not stand in the way of this,” according to the administration. However, the American Academy of Pediatrics, the American Federation of Teachers, the National Education Association, and the School Superintendents Association don’t agree.
“Educators and pediatricians share the goal of children returning safely to school this fall. Our organizations are committed to doing everything we can so that all students have the opportunity to safely resume in-person learning.
We recognize that children learn best when physically present in the classroom. But children get much more than academics at school. They also learn social and emotional skills at school, get healthy meals and exercise, mental health support and other services that cannot be easily replicated online. Schools also play a critical role in addressing racial and social inequity. Our nation’s response to COVID-19 has laid bare inequities and consequences for children that must be addressed. This pandemic is especially hard on families who rely on school lunches, have children with disabilities, or lack access to Internet or health care.
Returning to school is important for the healthy development and well-being of children, but we must pursue re-opening in a way that is safe for all students, teachers and staff. Science should drive decision-making on safely reopening schools. Public health agencies must make recommendations based on evidence, not politics. We should leave it to health experts to tell us when the time is best to open up school buildings, and listen to educators and administrators to shape how we do it.
Local school leaders, public health experts, educators and parents must be at the center of decisions about how and when to reopen schools, taking into account the spread of COVID-19 in their communities and the capacities of school districts to adapt safety protocols to make in-person learning safe and feasible. For instance, schools in areas with high levels of COVID-19 community spread should not be compelled to reopen against the judgment of local experts. A one-size-fits-all approach is not appropriate for return to school decisions.
Reopening schools in a way that maximizes safety, learning, and the well-being of children, teachers, and staff will clearly require substantial new investments in our schools and campuses. We call on Congress and the administration to provide the federal resources needed to ensure that inadequate funding does not stand in the way of safely educating and caring for children in our schools. Withholding funding from schools that do not open in person fulltime would be a misguided approach, putting already financially strapped schools in an impossible position that would threaten the health of students and teachers.
The pandemic has reminded so many what we have long understood: that educators are invaluable in children’s lives and that attending school in person offers children a wide array of health and educational benefits. For our country to truly value children, elected leaders must come together to appropriately support schools in safely returning students to the classroom and reopening schools.”